Prostate Cancer
What is Prostate Cancer?
The prostate gland is a secretory gland situated around the bladder neck, and it releases seminal fluid to transport sperm.
Amongst malignancies that affect men, Prostate Cancer is one of the most common types. The overall 5- year survival rate for this cancer is greater than 95%.
While many men die “with” prostate cancer rather than “of” prostate cancer it is important to note that more men die of prostate cancer each year in Australia than women die of breast cancer.
Who Does Prostate Cancer Affect?
Prostate Cancer occurs only in men and is more common in men who are older than 50 years, but it can occur in younger men, especially if there is a strong family history. Therefore, testing for prostate cancer should begin at age 50, or from 40-45 years of age depending on risk factors.
Positive family history on the father’s side of the family (father, paternal uncles, brothers) is the main risk factor and is more likely to result in more advanced cases of malignancy.
Also, a strong family history of breast, ovarian or pancreatic cancer may indicate the presence of a BRCA gene defect which is another risk factor.
The rate of prostate cancer also varies with race, with Asians having the lowest incidence, the Caucasians Hispanics and Blacks having higher incidence rates. However, Asians who have adopted the Western lifestyle have been shown to carry a higher risk of prostate cancer.
What are the Causes of Prostate Cancer?
The causes of Prostate Cancer are still not fully understood. Genetic and racial factors play a role as do dietary factors such as a high-fat diet and obesity.
What are the Symptoms of Prostate Cancer?
The symptoms don’t appear in earlier stages of the disease. Therefore, men should not rely on symptoms as a guide as to whether there is anything wrong. A PSA test and a prostate examination are the usual tests used to screen for prostate cancer.
As the malignancy progresses, it can cause the following symptoms:
- Difficulty in urination, the need to push harder
- A weaker stream of urine
- Pelvic discomfort
- Blood observed in ejaculation (semen)
- Erectile Dysfunction
- Infertility
- Fatigue,
- Weight loss,
- Bone Pain
Types of Prostate Cancer
Prostate cancer occurs when a tumour develops in the prostate gland. A core distinction with Prostate Cancer is whether the Cancer:
- is localised only in the Prostate, or
- if it has spread outside the prostate gland to the lymph nodes, bones, or other areas. This is called metastatic prostate cancer.
The most common type of prostate malignancy is adenocarcinoma, either acinar or ductal in nature (almost 98% of all cases).
Other rare types include neuroendocrine (small cell) cancers, sarcomas and others (roughly 1% of all cases).
Gleason Score for Prostate Cancer
Historically, a scale called Gleason score is used for this which gives a score out of 10.
The Prostate Cancer can be graded based on its aggressiveness and spread.
Oddly, the lowest possible number is a score of 6 which means the cancer is low grade. A score of 7 indicates intermediate cancer, and scores of 8-10 mean it’s very aggressive.
The Gleason score is now being replaced with a simpler system called the ISUP (International Society of Uropathologists) classification.
This system is based on the Gleason score as follows:
- ISUP 1 - Gleason Score 3+3 = 6
- ISUP 2 - Gleason 3+4 = 7
- ISUP 3 - Gleason 4+3 = 7
- ISUP 4 - Gleason Score 8
- ISUP 5 - Gleason Score 9,10
Nowadays, ISUP is preferred due to it simplicity and less anxiety to patients.
TNM Staging of Prostate Cancer
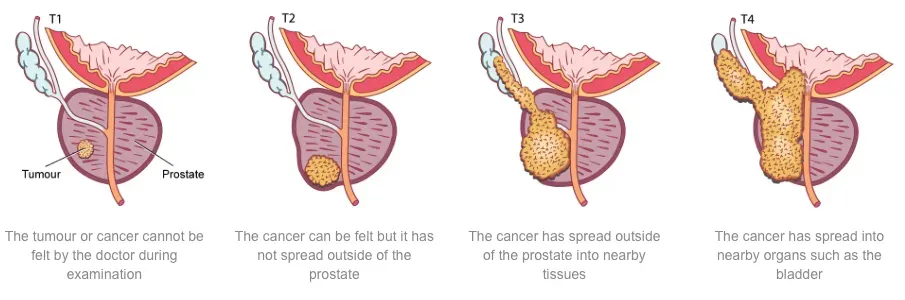
TNM staging essentially describes how far cancer has spread within and/or beyond the prostate capsule. In cases where there are no distant secondaries and where curative treatment is being considered, the T stage is particularly important:
- T1: Tumour is confined within the prostate and the prostate feels normal. It is usually diagnosed on the basis of a raised PSA.
- T2: Tumour is confined to the prostate but the prostate feels irregular to examination
- T3: Tumour has spread just beyond the shell of the prostate into nearby tissue and/or the seminal vesicles at the back of the prostate gland.
- T4: Tumour has spread into adjacent organs such as the bladder, rectum, or pelvic sidewall.
Prostate cancer can also spread to lymph nodes (N stage) and to other parts of the body such as to bone and other organs as metastases (M stage).
It is important to note that prostate cancer does not typically produce symptoms until it is advanced. This is why it is important for men to get PSA tests as this is the main way that prostate cancer will be diagnosed before it has spread.
How is Prostate Cancer Diagnosed?
Prostate cancer foundation of Australia (PCFA) and Cancer Council Australia recommends regular PSA screening of healthy men over the age of 50. Earlier PSA screening at the age of 40 is recommended if the risk of prostate cancer is increased (ie family history), as the early prognosis is crucial for a more positive outcome.
Some men present with urinary symptoms that could be related to prostate cancer. However, these symptoms are much more likely due to enlarged prostate (BPH) unless prostate cancer is at an advanced stage.
Screening involves
- a Prostate-Specific Antigen (PSA) Test and possibly
- a Digital Rectal Examination
If these tests yield abnormal results, to confirm malignancy and its stage Dr Hadley will consider any of the tests listed below:
- Multiparametric prostate MRI
- Prostate Biopsy
- Cystoscopy
- Urinary Flow or Urodynamic Testing
- Other Imaging Tests
Prostate-Specific Antigen - PSA Test
Prostate-Specific Antigen is a substance produced almost exclusively in the prostate and plays a role in fertility.
The vast majority is actually released into the ejaculate but tiny amounts are released into the bloodstream and can be detected by a simple blood test. Abnormally high levels of PSA can be an indication of disease of the prostate.
Common reasons for a high PSA level in the bloodstream may include:
- Prostate cancer,
- Large prostates
- Infection of the prostate
- Ejaculation, or cycling
Obviously, the first concern is to exclude prostate cancer. Urologist review is advised to exclude this.
Digital Rectal Examination (DRE)
The bladder is the organ that stores urine and the urethra is the tube that drains urine out through the penis. The prostate lies immediately beneath the bladder and completely surrounds the urethra and lies immediately in front of the rectum (back passage).
Dr Hadley would normally perform a Digital Rectal Examination (examination via the back passage) of the prostate, an otherwise inaccessible internal organ.
During a Digital Rectal Examination, Dr Hadley gently inserts a gloved finger into the rectum to feel the condition of the prostate that lies close to the rectal wall. If he feels something suspicious such as a lump or bump, further tests will be carried out.
Age-related enlargement is not a particular concern but if the gland feels abnormally firm or hard, it may sometimes be an indication of abnormal growth in the prostate gland.
Dr Hadley will discuss the test results with you. If anything suspicious is detected such as a lump or irregularity during the exam, further tests will be required.
After the test, you may continue your normal activities.
Prostate Biopsy
This test is commonly performed because either a blood test called PSA is abnormally high or the Digital Rectal Examination (DRE) of the prostate is abnormal. More commonly nowadays biopsy is performed after MRI of the prostate shows suspicion of prostate cancer.
There are mainly two approaches.
Transrectal biopsy
This was the most commonly performed technique. The biopsy needle is passed through the rectum into the prostate. It is quicker and does not need a general anaesthetic. However, due to the risk of serious infective complications, Dr Hadley does not advocate for this.
Transperineal biopsy
This new technique involves passing the biopsy needle through the perineum which is the area between the scrotum and the anus. This approach is associated with less infection and allows easier sampling in the anterior part of the gland. In addition, more cores can be taken compared to the transrectal biopsy which means that the results can potentially be more accurate. However, it often involves a general anaesthetic, takes longer and may be associated with more short-term urinary flow problems.
Dr Hadley performs prostate biopsies in many different ways. In some cases he may need to organise an MRI guided biopsy for small lesions in difficult places. This involves putting a needle into a small lesion under MRI guidance. This is very expensive, but also very accurate, so is only performed under certain circumstances.